|
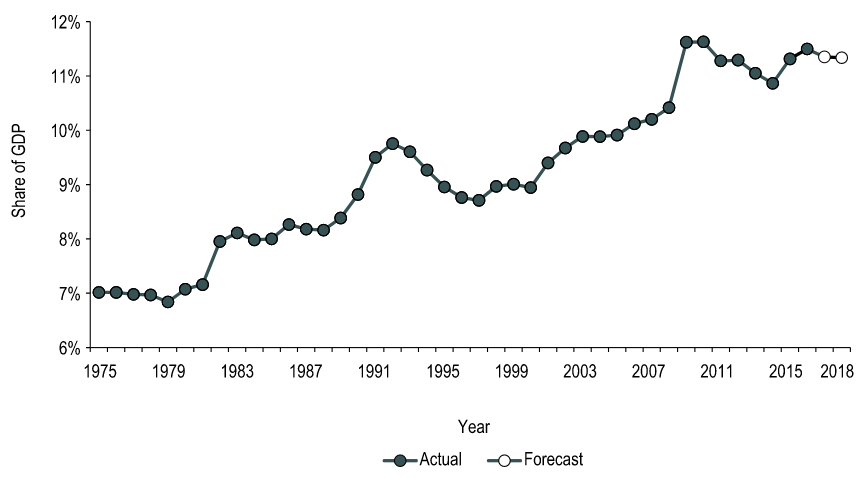
By: Victoria Lee-Kim, Meds 2022 QMed LEAD provided Queen’s medical students with the opportunity to hear from Don Drummond on the topic of healthcare economics and the growing national health expenditures. For those of you who are unfamiliar with him, he is a renowned Canadian economist who served in the federal Department of Finance, a professor at Queen’s School of Policy Studies, and was a Chief Economist at TD bank. His talk got me thinking—why isn’t healthcare economics more integrated into our medical education? We have diverse and strategic student minds that may eventually be able to combine their medical knowledge with policy, and may even be able to tackle the Canada’s growing health expenditure problem. Here are some of the striking statistics and insightful ideas he introduced, mixed with thoughts of my own: According to the Canadian Institute for Health Information (CIHI), in 2018, total health expenditure in Canada reached $253.5 billion (a growth of approximately 4.2%). That is 11. 3% of Canada’s gross domestic product. Also, approximately $6839 per person. To put that into context: using the Organization for Economic Co-operation and Development (OECD) statistics, Canada is above the OECD country average in terms of healthcare spending as a percentage of GDP and per-person healthcare spending. But why are we spending more than the average? Even accounting for the population spread over a massive amount of land, our split between public and private health care spending should theoretically equate to us spending less on healthcare. Our public-sector share of total health expenditure is 70% (30% private) which is below the average of 73%. For more context, the United States healthcare system is 82 % publicly-funded and 18% private. Canada is one of the top spenders, yet we constantly fall short in rankings of international health systems. If you ask me, something doesn’t quite seem to add up! Overall in Canada, the health-to-GDP ratio has trended upward in the last 40 years for reasons including general inflation, population growth, aging, novel drugs and infrastructure (Figure 1). Hospitals, drugs, and physician services make up the largest shares of health expenditures. In 2018, the annual growth forecast was 3.7%. We have to think of this trend while we practice medicine! The aging of the Baby Boomer generation will demand more of physicians, which means more hours per person or more people to compensate. Compensation currently accounts for more than 60% of hospital budgets, and thus is a huge cost driver. Moreover, old infrastructure must be replaced and increasingly expensive prescriptions are becoming the norm. The introduction of high-cost medicines can increase prescribed drug spending. These changes are predictable, but the issue is that our governments work in four year blocks, making it next to impossible to create systemic changes that will match the growth of healthcare expenditures. Figure 1. How health spending has changed in Canada over the last 40+ years; https://www.cihi.ca/en/health-spending/2018/national-health-expenditure-trends/how-has-health-spending-growth-changed-over-the-last-40-years You’re probably thinking “Ok… so what? What can we do?” Well, I’m obviously no expert and am aware that my opinion doesn’t hold a lot of weight, but I think awareness of these statistics is a good place to start! Awareness introduces an economic perspective into our future decisions as physicians. It can play a part in our willingness to provide preventive medicine, can help guide our choices of diagnostic tests , and help us decide which policies to advocate for. Who knows, maybe a QMed graduate will be at the forefront of systemic change that improves our healthcare system on a macro level! References
0 Comments
|
 RSS Feed
RSS Feed
